Archives of Community Medicine and Public Health
Primary Healthcare Service Delivery during an Active Conflict: The 2023 Israel-Hamas War
1Department of Emergency Medicine, University of California, Davis, Sacramento, California, USA
2Project HOPE: The People-to-People Health Foundation, Washington, DC, USA
3Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam-si, Gyeonggi-do, South Korea
4Department of Emergency Medicine, Harbor-UCLA Medical Center, Torrance, CA, USA
Author and article information
Cite this as
Shetty PP, Jeong J, McMillan A, Badwan M, May S, Latifi C. Primary Healthcare Service Delivery during an Active Conflict: The 2023 Israel-Hamas War. Arch Community Med Public Health. 2025;11(3):049-053. Available from: 10.17352/2455-5479.000223
Copyright License
© 2025 Shetty PP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Abstract
In December 2023, Project HOPE, an international humanitarian aid organization, opened a primary healthcare clinic in Deir al-Balah, Gaza. The clinic was created in response to increased population healthcare needs during the 2023 Israel-Hamas war. This article describes the startup and case mix from the Project HOPE primary healthcare clinic in Deir al Balah, Gaza, between December 2023 and June 2024. Opening the clinic required navigating several logistical, administrative, security, and technical challenges common to humanitarian contexts. Over six months, the clinic conducted over 24,000 patient consultations. Major morbidities included those due to communicable diseases (such as upper respiratory tract infections, skin diseases, and acute watery diarrhea) as well as obstetric visits. Visits due to trauma and chronic diseases made up a low proportion of visits. Children between 6 months and 5 years of age and pregnant and lactating women were also assessed for their nutritional status using mid-upper arm circumference measurement. Prevalence of malnutrition varied over the study period, with percentages in children increasing, while those in pregnant and lactating women decreased. Indirect morbidity and mortality due to lack of access to healthcare services during conflict is an often under-reported issue, and Project HOPE’s reported experience in the Deir al Balah clinic may help to inform subsequent health interventions in Gaza and in other conflict-affected settings.
Introduction
The ongoing conflict in Gaza has had devastating effects on the existing healthcare system and severely compromised its ability to provide essential healthcare services to the population [1]. As of December 4th, 2024, the World Health Organization (WHO) reports only 47% of hospitals and 37% of primary healthcare facilities as partially or fully functional; this is combined with significant increases in health needs due to injuries, reproductive health issues, malnutrition, chronic diseases, and other morbidities [2]. Even for humanitarian aid groups accustomed to working in conflict settings, delivering needed supplies and services in Gaza has been particularly challenging and severely limited [3].
The effects of armed conflict on health are well described; this includes direct health effects such as morbidity and mortality due to trauma, as well as indirect health effects due to displacement, loss of shelter, breakdown of public health infrastructure, lack of access to healthcare services, and food insecurity, among various other causes [4-6]. Health consequences include excess morbidity and mortality due to increases in infectious diseases [7], non-communicable diseases [8-10], sexual and reproductive health [11,12] and mental health [13], among others. Delivery of essential healthcare in conflict settings is often compromised, and re-establishing Primary Healthcare (PHC) services is necessary to address this increased burden of disease [14].
Project HOPE is an international humanitarian organization whose mission is centered on delivering critical humanitarian aid and support to regions facing severe crises. Before the conflict, Project HOPE had no active presence in Gaza but maintained a well-established program in Egypt, which emerged as a key hub for organizations supporting Gaza. Leveraging relationships in Egypt, Project HOPE initially facilitated the import of medical supplies and materials through the critical Rafah crossing into Gaza. This effort expanded to include the establishment of a primary healthcare clinic in Deir al Balah to provide medical care and help address growing humanitarian needs in the region.
This article describes the startup and case mix from the Project HOPE primary healthcare clinic in Deir al Balah, Gaza, between December 2023 and June 2024.
Methods
Study setting
Project HOPE initially sent two expatriate health staff into Gaza (a trauma specialist and a reproductive health specialist/midwife), facilitated by the Emergency Medical Team Coordination Cell (EMTCC), and subsequently hired local physicians and nurses to initiate primary health care services. The first clinic was opened on December 9th, 2023, in Deir al Balah, repurposing a former dentist’s office. Due to import restrictions and bureaucratic challenges, Project HOPE was unable to bring in medical supplies until January and relied on donations of pharmaceuticals and supplies from other international non-governmental organizations (NGOs) to support clinic operations. Deir al Balah was chosen due to the lack of humanitarian actors in the area and a high proportion of internally displaced persons (IDPs) within the catchment population. In late January 2024, an adjoining space was opened to accommodate a separate sexual and reproductive health (SRH) clinic. Overall services included the provision of general primary and reproductive healthcare, including management of chronic disease; however, routine vaccinations were not available during this reporting period.
Data collection
Basic patient-level data were captured in the clinic using a line-list format; data collected included demographic information, mid-upper arm circumference (MUAC) for children and Pregnant and Lactating Women (PLW), pregnancy status, patient diagnosis, and treatment provided. This line list was transcribed to an Excel file for analysis and reporting purposes. Patient diagnoses were subsequently categorized into a standard diagnostic category listing used by Project HOPE in emergency settings by a single author (AM) and verified by a second author (PS). Patient identity could not able to be determined through the data collection and analysis process; each patient was provided a unique identifier number on their first visit, and no other patient identifying information was available to the study authors.
Statistical analysis
A descriptive analysis was performed for all patients who visited the clinic during the 6-month study period (December 9th, 2023 – June 8th, 2024). Information related to visit status was collected: patients who visited once during the study period were coded as single visits, whereas those who visited two or more times were coded as multiple visits. When calculating proportional morbidity, patients with the same diagnostic category who were revisited within one week were excluded. MUAC measurements were used to evaluate the proportion of patients with acute malnutrition among children 6 months – 5 years of age and PLWs. To calculate the proportion of patients with an abnormal MUAC value, revisits were excluded. Data were analyzed using Stata 18.0 (StataCorp LLC; College Station, Texas, USA).
The UC Davis Institutional Review Board reviewed the research and determined that this study was exempt from IRB review (February 9th, 2024; Reference number: 2144852-1).
Results
Over the study period, a total of 24,126 patient consultations were conducted at the clinic; women made up 63.4% of visits. Median patient age was 26 years, and approximately one-third were children or adolescents. 73.7% of patients reported being internally displaced at the time of their visit. Pregnant women accounted for 13.1% of total visits, and 15.5% of visits were to the SRH clinic. Over 40% of consultations were for patients who visited the clinic two or more times (Table 1).
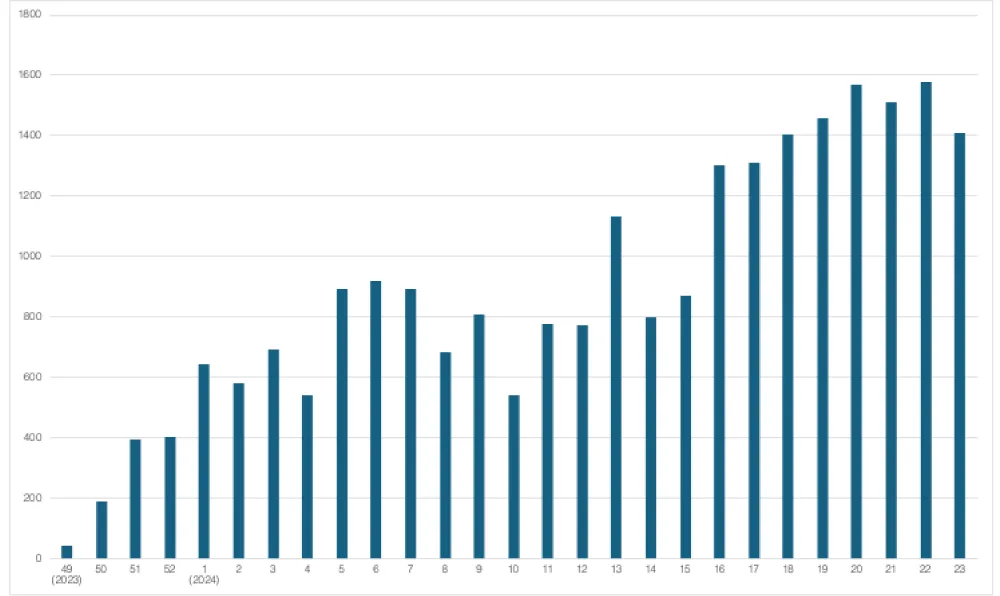
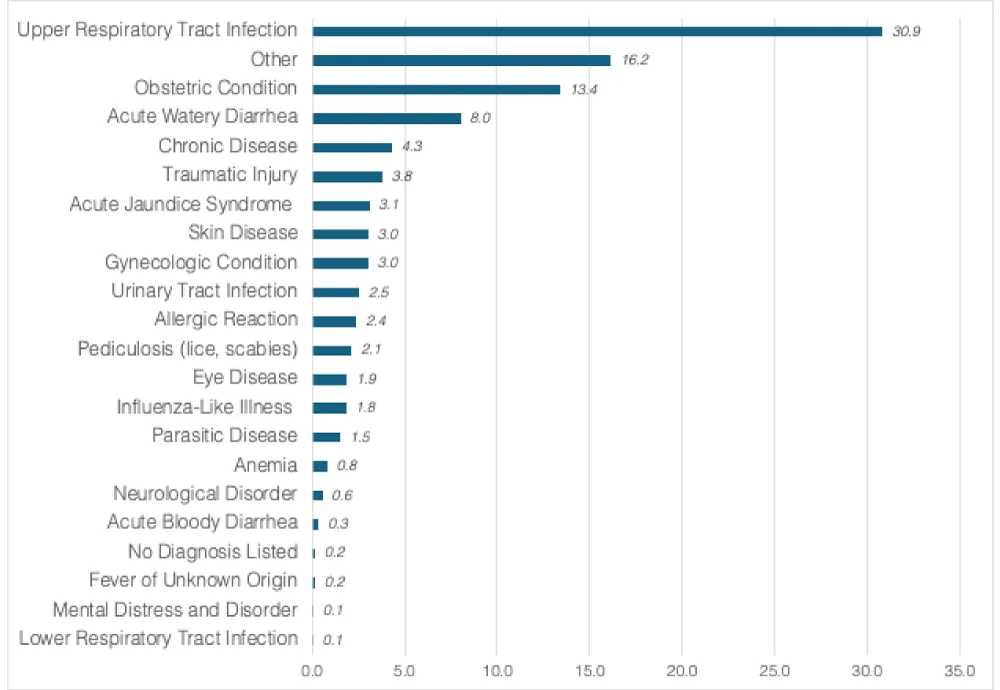
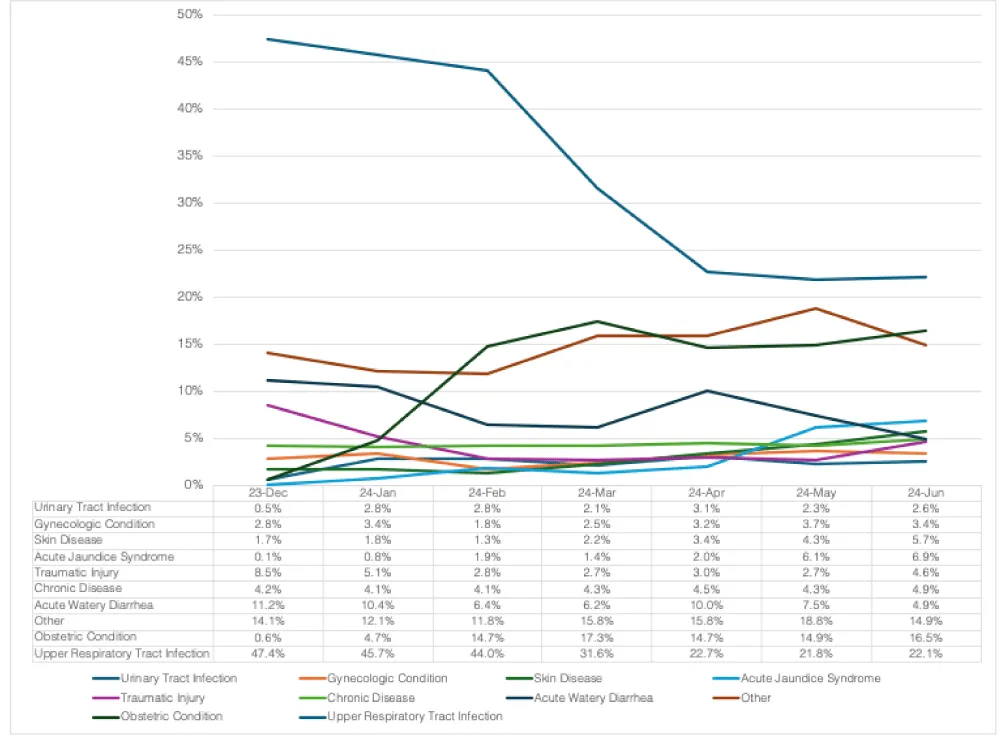
The number of patients who visited per epidemiological week steadily increased over the study period; from April 14th onward, over 1,200 consultations were made weekly (Figure 1). The five most common diagnostic categories were upper respiratory infection (URI), other diseases, obstetric conditions, acute watery diarrhea, and chronic diseases, which accounted for over 70% of all consultations (Figure 2). Over the study period, the proportion of URI cases gradually decreased, whereas the proportions of obstetric conditions, acute jaundice syndrome, and skin diseases increased (Figure 3).
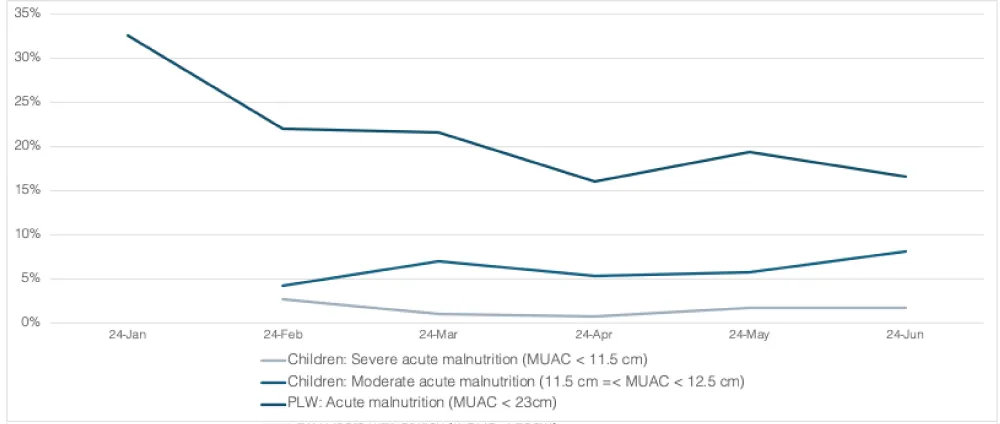
The proportion of children aged 6 months to 5 years with severe acute malnutrition (SAM) remained stable at 1% to 2%. However, the proportion of children with moderate acute malnutrition (MAM) increased slightly from 4.2% to 8.0% during the study period. Among PLWs, the proportion of patients with acute malnutrition showed a consistent decline, decreasing from approximately 32% to 16% (Figure 4).
Patients who visited the clinic multiple times were more likely to be women, older, pregnant, visitors to the SRH clinic, and diagnosed with obstetric conditions (Appendix Table 1). The top five specific morbidities seen in patients diagnosed with chronic disease were hypertension, diabetes mellitus, gastritis/GERD, arthritis, and respiratory disease (asthma or chronic obstructive pulmonary disease) (Appendix Table 2). The top five reasons seen in patients who presented for obstetric conditions were antenatal care, vaginitis, anemia, urinary tract infection, and family planning (Appendix Table 3).
Discussion
This report describes the startup and case mix from a Project HOPE-supported clinic in Deir al Balah, Gaza, over six months from December 9th, 2023, to June 8th, 2024. Initiation of healthcare services in conflict settings often requires significant adaptation to the context; this was experienced in Gaza, where staff needed to rapidly find a suitable clinic location, collect patient data by hand with subsequent digitization, manage frequent power outages, navigate significant security challenges, and provide services with limited resources, among other difficulties. These programmatic and operational challenges are not unique to Gaza and are common in conflict-affected settings [15].
Data from the clinic showed a high proportion of visits were due to communicable diseases (upper respiratory tract infections, skin diseases, acute watery diarrhea, etc.), while a few were due to trauma (3.8%). While traumatic injuries are commonly seen in conflict settings, the role of the Deir al Balah clinic as an outpatient primary healthcare center, as well as the relative proximity of an acute care hospital (Al-Aqsa Hospital), likely contributed to the low frequency of visits for traumatic conditions. A low proportion of visits were due to non-communicable or chronic diseases as well (4.3%), with the majority of these due to visits for hypertension and diabetes management. Most (73.7%) of visits were from patients who were internally displaced, which exemplifies the effect of the conflict on population movement. We also found that 44.7% of visits were follow-up visits; while a higher percentage may be expected in a conflict setting with limited access to pre-existing PHC services, population displacement, and competing priorities for patients may have played a role in this.
There were an estimated 50,000 pregnant women in Gaza as of May 2024, with little access to specialized obstetric services [16]. This service gap was observed within the clinic; the percentage of visits for an obstetric condition increased from 4.7% to 14.7% within the first month of SRH service provision. The prevalence of global acute malnutrition within children 6 months to 5 years also increased over the study period, primarily within those with MAM (4.2% to 8.0%). A recent cross-sectional nutrition survey demonstrated a higher rate of SAM (6.7%) and a similar rate of MAM (9.6%) throughout the country, indicating a precarious nutritional situation in Gaza [17]. Interestingly, the proportion of PLWs with acute malnutrition decreased, possibly reflective of the fact that most patients who attended the SRH clinic were repeat/follow-up visits and were provided nutritional supplementation when initially diagnosed with malnutrition.
Several key lessons were learned by Project Hope in the startup of the Deir al Balah clinic. First, rapid deployment of expatriate staff with a quick and purposeful transition to local staffing, along with the repurposing of existing infrastructure, allowed for service delivery to commence in a timely fashion. Second, reproductive and maternal health care are important to offer from the onset of a crisis; we saw rapid uptake and return visits for these services within a short period of time. Third, systematic nutrition monitoring, even if not providing therapeutic care, is essential to inform the overall humanitarian response. Lastly, PHC clinics generally need to prepare for a wide range of patient needs, but even in conflict settings, morbidity due to communicable diseases may present the highest burden of disease, especially in contexts where public health infrastructure is compromised.
During an active conflict, indirect morbidity and mortality due to various factors, including lack of access to essential health services, are likely much higher than direct mortality due to trauma [18]. While provision of healthcare services from international and local organizations may act as a stopgap measure, continued conflict in Gaza will only result in worsening health outcomes and a fragile health sector, which will be extremely difficult to rebuild [19]. Project HOPE’s experience in the Deir al Balah clinic, as reported in this study, may help to inform subsequent health interventions in Gaza and in other conflict-affected settings.
Limitations
There are several limitations to this study. This data only represents the experience and case-mix from one clinic, which may not be representative of the situation throughout Gaza or other conflict settings. The dataset includes only those able to access the clinic, which may exclude vulnerable populations who couldn’t travel to the clinic or were unaware of the offered services. Similarly, the reported prevalence of acute malnutrition is based only on those who presented to the clinic; thus, an inherent selection bias is present. Detailed descriptions of patients’ clinical status were not available, and diagnoses were aggregated into broad categories that do not fully represent the nuances of patient morbidities.
References
- World Health Organization. oPt Emergency Situation Update: 7 Oct 2023 – 4 Dec 2024. Published 2024 Dec 4. Available from: https://www.emro.who.int/images/stories/Sitrep_52.pdf
- World Health Organization. oPt Emergency Situation Update: 7 Oct 2023 – 25 Sep 2024. Published 2024 Sep 25. Available from: https://www.emro.who.int/images/stories/Sitrep_46b.pdf?ua=1
- Neuman S, Baba A. Delivering aid in a war zone is always difficult. In Gaza, it's proving even harder. National Public Radio. Available from: https://www.npr.org/2023/12/09/1217767373/gaza-humanitarian-aid-refugees-war-israel-hamas
- Armed conflict and public health: into the 21st century. J Public Health (Oxf). 2020;42(3):e287–e298. Available from: https://doi.org/10.1093/pubmed/fdz095
- Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88. Available from: https://doi.org/10.1016/s0140-6736(18)32203-7
- Murray CJL, King G, Lopez AD, Tomijima N, Krug EG. Armed conflict as a public health problem. BMJ. 2002;324(7333):346–9. Available from: https://doi.org/10.1136/bmj.324.7333.346
- Ghobarah HA, Huth P, Russett B. The post-war public health effects of civil conflict. Soc Sci Med. 2004;59(4):869–84. Available from: https://doi.org/10.1016/j.socscimed.2003.11.043
- Aebischer Perone S, Martinez E, du Mortier S, Rossi R, Pahud M, Urbaniak V, et al. Non-communicable diseases in humanitarian settings: ten essential questions. Confl Health. 2017;11:17. Available from: https://doi.org/10.1186/s13031-017-0119-8
- Gebrehiwet TG, Abebe HT, Woldemichael A, Gebresilassie K, Tsadik M, Asgedom AA, et al. War and health care services utilization for chronic diseases in rural and semiurban areas of Tigray, Ethiopia. JAMA Netw Open. 2023;6(8):e2331745. Available from: https://doi.org/10.1001/jamanetworkopen.2023.31745
- Jawad M, Vamos EP, Najim M, Roberts B, Millett C. Impact of armed conflict on cardiovascular disease risk: a systematic review. Heart. 2019;105(18):1388–94. Available from: https://doi.org/10.1136/heartjnl-2018-314459
- Urdal H, Che CP. War and gender inequalities in health: the impact of armed conflict on fertility and maternal mortality. Int Interact. 2013;39(4):489–510. Available from: https://doi.org/10.1080/03050629.2013.805133
- O’Hare B, Southall D. First do no harm: the impact of recent armed conflict on maternal and child health in sub-Saharan Africa. J R Soc Med. 2007;100(12):564–70. Available from: https://doi.org/10.1177/0141076807100012015
- Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights. 2015;15:29. Available from: https://bmcinthealthhumrights.biomedcentral.com/articles/10.1186/s12914-015-0064-9
- Sondorp E, Bornemisza O. Primary health care and armed conflict. J R Soc Promot Health. 2004;124(6):251–2. Available from: https://doi.org/10.1177/146642400412400606
- Omam LA, Jarman E, O'Laughlin KN, Parkes-Ratanshi R. Primary healthcare delivery models in African conflict-affected settings: a systematic review. Confl Health. 2023;17:34. Available from: https://doi.org/10.1186/s13031-023-00533-w
- World Health Organization: Health Cluster. Hostilities in the occupied Palestinian territory (oPt): Public Health Situation Analysis (PHSA). 2024. Available from: https://www.un.org/unispal/wp-content/uploads/2024/05/WHO-PHSA-oPt-020524-FINAL.pdf
- Albelbeisi A, Zinszer K, El Bilbeisi AH, Abuzerr S. The burden of acute malnutrition among children under five in conflict-afflicted Gaza Strip: prevalence and associated factors. Front Nutr. 2024;11:1478485. Available from: https://doi.org/10.3389/fnut.2024.1478485
- Stamatopoulou-Robbins S. The human toll: indirect deaths from war in Gaza and the West Bank, October 7, 2023 forward. Watson Institute for International & Public Affairs: Costs of War Project; 2024. Available from: https://watson.brown.edu/costsofwar/files/cow/imce/papers/2023/2024/Costs%20of%20War_Human%20Toll%20Since%20Oct%207.pdf
- Blanchet K, Najem M, Shadid L, Ali Fehmi R, Al Hammouri F, Saed G, et al. Rebuilding the health sector in Gaza: alternative humanitarian voices. Confl Health. 2024;18:42. Available from: https://conflictandhealth.biomedcentral.com/articles/10.1186/s13031-024-00599-0


 Save to Mendeley
Save to Mendeley

